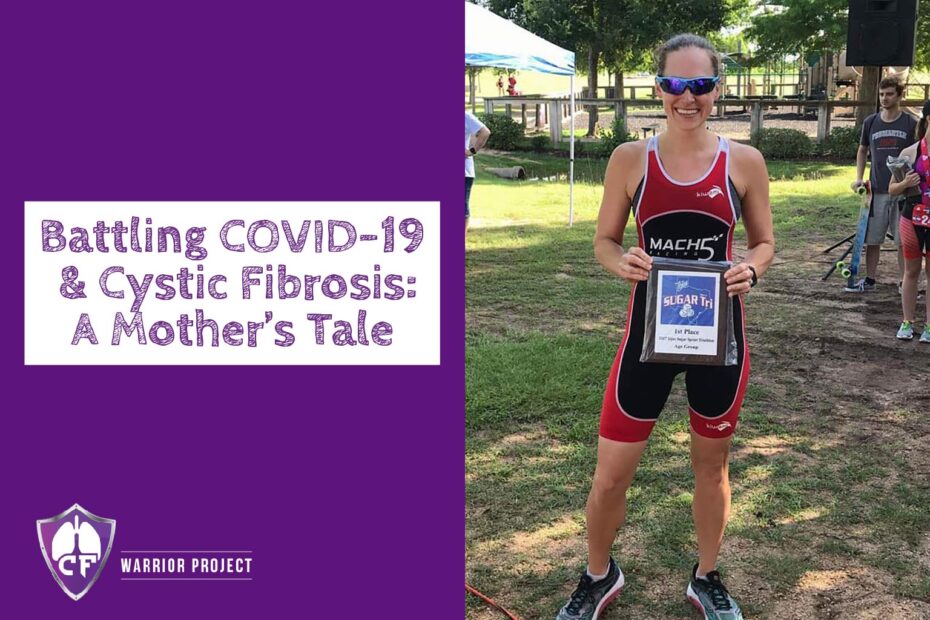
Debra Sanchez is a 35-year old married mother of two. Debra is a fantastic athlete who started swimming competitively when she was just 10 years old and continued through high school. She played club water polo at Baylor University. While at Baylor, she was diagnosed with cystic fibrosis (CF). The diagnosis motivated her to start running. She has completed two full Ironmans (2.4mi swim, 112mi bike, 26.2mi run), 7 half Ironmans (1.2mi swim, 56mi bike, 13.1mi run), and numerous marathons and half-marathons.
She was on the CFTR modulator Kalydeco but she stopped it once she was pregnant with her second child in 2018. Her doctor wanted to keep her off of Kalydeco while she was breastfeeding, and she didn’t see any significant changes while on the drug so her doctor kept her off of it.
Here is Debra’s COVID account:
When my one-year old Luke developed a fever, we initially thought it was a reaction to his vaccines but the next day Levi, our four-year old, had a fever too and so we took Luke to get a COVID test and he was indeed positive. They said we should assume Levi was positive too and not to bring him in for testing. My husband Eddie showed symptoms the next day and took a test and was declared positive. I was the last one to develop symptoms. I knew I had it based on Luke and Eddie’s positive tests and my symptoms, but I wasn’t actually tested until I went to the ER nine days after the onset of my symptoms. As expected, the test came back positive.
Prior to contracting COVID-19 from my one-year old, I had already increased my normal CF breathing treatments, as I had been working from home since March. I figured, since I’m already home, I might as well do the extra treatments and get my lungs in the best possible shape in case I do get sick.
My COVID-19 symptoms started with fever, stabbing headaches, fatigue, body aches and coughing. About a week after the onset of my symptoms, my cough continued to get worse, to the point where my O2 (oxygen) was steadily dropping each day, and I was unable to speak without constant, painful coughing. My doctor and I both agreed I should try to fight COVID at home if possible, and I continued checking my O2, knowing that if it dropped below 90, I would go in.
Nine days after my symptoms started, I woke up with an O2 of 88 and I was struggling to breathe. I was crying for my husband to plug in my nebulizer compressor because I couldn’t get down to do it myself.
I was terrified to go into the hospital because I knew COVID patients were not allowed to do nebulized breathing treatments, and I knew I would be completely alone. At this point, I had no other choice. I hugged my sons goodbye, told them how much I loved them, and prayed I would be back to see them soon.
I waited in the ER for nine hours before a room became available. While there, they did an X-ray that showed double pneumonia, partially collapsed lungs, and a secondary infection from COVID. They started me on IV antibiotics and O2 immediately. My CF doctor and the ER staff advised I would need a negative pressure room in order to do breathing treatments, and those are ‘few and far between’ – not to mention regular rooms were all full as well. I finally got a room, and even then I wasn’t sure if I’d be allowed to do breathing treatments, which terrified me. I needed them to breathe on a good day, and especially now.
When the respiratory therapist finally brought me my breathing treatments, I cried. They put a plastic tent over me – which was hot and suffocating – but I was so thankful that I was able to do treatments. No one was allowed to enter my room for an hour after treatments.
I continued to get worse before I got better. The day before my symptoms started, I ran nine miles while pushing my son in the stroller. Now I could not walk 10 feet to the bathroom. I called a nurse to help me, made it to the toilet, but the short walk sent me into a coughing fit and I could not stop coughing or catch my breath long enough to use the restroom, so she helped me back to bed – where I sat, unable to breathe, unable to stop coughing, and still needing to use the restroom.
The next morning, doctors advised I would be getting convalescent plasma, which finally arrived at 1:00 A.M. There was a shortage of plasma at the blood bank on site, so it had to be brought in from somewhere else. I had no energy to watch TV or look at my phone most of the day. I was on Cefepime IV every 8 hours, Tobramycin IV every 24 hours, nebulized meds every 4 hours, blood thinner shots every 12 hours, vital checks every 4 hours, and in between I was lying prone as much as possible to try and help my lungs.
They did a CT scan to make sure I did not have any blood clots in my lungs. Results showed no clots, but a significant amount of inflammation/pneumonia. I have a follow up CT in 3 months to check for permanent lung damage and/or scarring. I also have a cardiologist appointment in a couple of weeks, as I’ve been having issues with tachycardia (excessive heart rate), and COVID has been linked to heart problems. I need to get my heart checked out before returning to my normal workout routine.
Being isolated in the hospital was terrible. I was there for seven days. I am used to having to advocate for myself, but it’s so difficult while struggling to speak (from coughing so much) and while I was already so fatigued.
The hospital was full of patients and short on staff because so many of their nurses were out with COVID. They were forced to bring in traveling nurses to help. Additionally, since everyone is alone, things that family members could typically help with, were now up to nurses. For example, they brought in a vest for me to use while I was asleep, but I had to call a nurse to plug it in because I couldn’t get out of bed to plug it in myself.
I keep hearing people say, “Everyone is going to get COVID eventually,” and perhaps that’s true, however; I strongly believe everyone should protect themselves as much as possible. No one knows how it will affect them, and our hospitals are especially strained right now. Additionally, we are still learning about COVID-19. The information seems to change daily, so the longer people are able to stay healthy and the more we are able to learn, the better our chances are for recovery.
Please stay safe!
Author’s note: Debra has no idea who in her family contracted the virus first and where they could have gotten it. She says that her family has always been very careful but they have had to make trips to pediatrician’s offices and places like that so they realize there is always risk even though the entire family wears masks and practices social distancing when they are out. Her health is much better than it was a few weeks ago, but nowhere near back to her normal. Her lung function is down and not back to baseline yet, but that is to be expected. Her left lung is still painful. Her CF doctor said her lungs will probably feel different for a long time. Her energy level is good, and she has started walking and even jogging. She is up to jogging half-a-mile at a time, so she has a long way to go with regards to getting her fitness back. She read studies about the benefits of CF modulators when dealing with COVID-19, so she started Kalydeco again after she was discharged from the hospital a couple weeks ago. She has also officially tested negative for COVID-19 and is back with her family. Debra is the only one still battling lasting effects from the virus. We wish her a full recovery.
Debra is an amazing woman in so many ways! To see her go through this was heartbreaking – so so glad she is on the other side of this and prayers she has no lingering issues.
Comments are closed.